The correlation between your monthly period and the pain that accompanies it is usually a pretty common occurrence. However, for some women, that pain can be especially excruciating and may not be resolved from taking over-the-counter medications typically recommended for menstrual pain.
Painful periods are a highly common problem among women and can keep women from being able to function in their daily lives due to their severe symptoms and discomfort.
Dysmenorrhea is the term for this medical gynecological disorder, which translates to difficult or painful periods. While menstrual abdominal cramps normally occur during the first few days of the period cycle, severe pain that persists and gets in the way of normal daily routines can be an indication of dysmenorrhea.
There are two kinds of dysmenorrhea that can occur: primary and secondary. Primary dysmenorrhea is oftentimes the most common gynecologic problem that occurs in women and not due to any underlying gynecologic disorder.
This kind of dysmenorrhea is commonly characterized by severe abdominal cramping pain that can begin before the onset of your period and last about 2-4 days. It is most likely to affect adolescents and usually improves as they mature. While primary dysmenorrhea can be quite painful, it is not harmful to the female body.
Secondary dysmenorrhea, on the other hand, is usually an indicator of an underlying gynecological problem. Most of the time, these disorders can be easily treated as long as they are identified. This type is most likely to affect adult women and is characterized by menstrual pain that contributes to an overarching medical condition.
Signs and Symptoms
The biggest indicator of dysmenorrhea is pain that results from menstruation. This pain can occur in the lower abdomen, lower back, hips, or thighs, and typically starts shortly before or during the period cycle and improves after a couple of days [1].
The pain can be dull or throbbing, and sometimes other symptoms are present, including nausea, vomiting, diarrhea, lightheadedness, and achiness. The pain that develops usually peaks within the first day or two of the period. Some women may also feel the need to urinate more frequently.
Dysmenorrhea that begins after the age of 25, as well as having no history of previous menstrual pain, can be an indicator of secondary dysmenorrhea. Also, pelvic abnormality upon physical examination points to secondary dysmenorrhea.
Having no response to treatments with nonsteroidal anti-inflammatory drugs or oral contraceptives is an indication there is an underlying medical condition that needs to be treated.
Causes
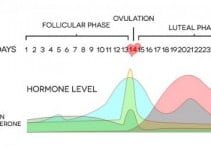
While the exact etiology of dysmenorrhea is not completely known, it is believed that primary dysmenorrhea is caused by excessive levels of prostaglandins [2].
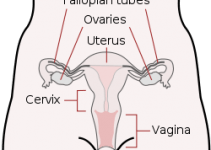
Prostaglandins are hormones that initiate uterine contractions throughout menstruation and childbirth, thereby resulting in the cramping pain that occurs in the abdominal section when the blood supply to the lining of the uterus is reduced.
Clots and pieces of bloody tissue from the uterine lining that passes through the cervix can contribute to the painful cramping that most women experience. A narrow cervical canal can increase the likelihood of experiencing such pain. High levels of prostaglandins can also contribute to the symptoms of nausea, diarrhea, and lightheadedness.
Secondary dysmenorrhea is thought to be brought on by a variety of medical conditions, such as fibroids (tumors within the uterine wall), adenomyosis, sexually transmitted infections, endometriosis, pelvic inflammatory diseases, ovarian cysts or tumors, and the use of intrauterine devices.
Since secondary dysmenorrhea is typically an indicator of an underlying gynecological disorder, it is common that a separate medical disorder is what causes it.
Treatments
Dysmenorrhea can be typically treated with medication or hormonal treatments. Primary dysmenorrhea is usually treated with analgesic medication. Over-the-counter nonsteroidal anti-inflammatory medication is usually recommended to help relieve the severe pain of menstrual cramping.
Women should begin taking the medication about 1-2 days before the onset of their period cycle in order to give it time to prevent menstrual cramping.
Over-the-counter medications can altogether help relieve the painful symptoms of dysmenorrhea and menstruation, as well as contribute to a lighter flow.
Hormonal treatment is another avenue of treatment for women with dysmenorrhea. Women can be prescribed oral contraceptive pills as well as other contraceptive hormonal treatments to help thin the uterine lining to decrease blood flow and lessen the intensity of cramping.
Oral contraceptives suppress ovulation and therefore lessen the impact of menstruation and blood flow. Continual hormonal treatment can prevent women from menstruating altogether while on the treatment.
There are also natural remedies that can be done to help lessen the symptoms of dysmenorrhea. Women can resort to a heating pad to help alleviate the painful cramping by placing it on their lower abdomen. Taking a warm bath, as well as massaging your abdomen, can also have positive effects on pain relief.
Exercise is another method that has been proven to relieve menstrual cramps for women, and so taking part in regular exercise can help significantly lessen the effects of dysmenorrhea.
Treatment for secondary dysmenorrhea can depend on the underlying medical condition, so consulting with a doctor to find out the primary cause of this dysmenorrhea is the first step in treating it.
References