Low platelet count is a common finding encountered during pregnancy and is only second to anemia [1] as the most common hematological abnormality during pregnancy. About one in ten pregnant women have this condition and it usually has no harmful effect on baby or mother.
What are platelets?
Platelets are plate-shaped cells derived from megakaryocytes in the bone marrow and normally live in the circulation for as long as 8-9 days. Their normal value ranges from 150,000 to 400,000 per microliter of blood.
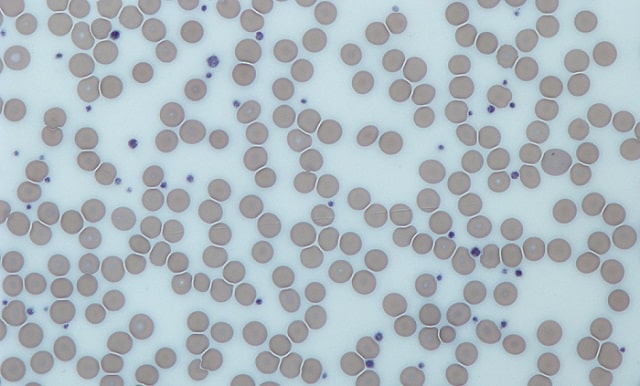
Image: wikimedia.org
If you have more than 400 million, the condition is called thrombocytosis. If you have fewer than 150 million it is known as thrombocytopenia.
Platelets play a critical initiating role in the blood clotting system. They create a blood clot and stops excessive bleeding, wherever blood vessel is injured.
Causes of low platelet count during pregnancy
There are 3 most common causes of low platelet count during pregnancy:
- Severe Headache
- Nausea & Vomiting
- Visual changes
- Abdominal Pain
- Dizziness
- Reduced urine output
- Rapid weight gain
1. Gestational Thrombocytopenia
Platelet counts between 100,000 and 150,000 per µL are typically caused by gestational thrombocytopenia and it accounts for 70%-80% of cases [2]. It occurs in the mid-second to third trimester. It may result from various mechanisms, including expanded intravascular volume and splenic as well as placental sequestration of platelets. The blood platelets can still perform their job, and will return to normal levels after your baby is born.
2. Preeclampsia
It is defined as blood pressure of greater than 140/90mmHg and proteinuria after 20weeks of gestation and accounts of 21% [2] of cases of thrombocytopenia at the time of delivery. It puts mother and the baby at high stake. Signs and symptoms of Preeclampsia include:
It is sometimes picked up by healthcare provider during antenatal checkups.
Preeclampsia may advance to Eclampsia which is an obstetrical emergency and is characterized by seizures and/or coma.
ITP or Immune thrombocytopenic Purpura
It is an autoimmune condition, occurring before pregnancy, where your immune system attacks the body’s platelets. It usually develops after a viral infection contracted during childhood. The chance of baby having thrombocytopenia also increases in ITP.
Other causes of low platelets count includes:
- HELLP Syndrome:
Characterized by Hemolysis, Elevated Liver enzymes and Low Platelet count is a life-threatening condition that can potentially complicate pregnancy. Some propose that it is a rare complication of Preeclampsia. - Medications: Heparin is a medicine used to treat abnormal blood clotting. This kind of thrombocytopenia is called Heparin-induced thrombocytopenia. Ibuprofen, paracetamol etc. can affect the platelet formation.
- Systemic Lupus Erythematosus (SLE): This is an autoimmune disorder in which the body attacks itself. Pregnancy may elevate the chances of SLE by forming antibodies that destroy various organs. It may target bone marrow, which is responsible for platelet formation. The affected bone marrow may cause low platelet count.
- Cancer: A pregnant woman may be affected with Myelodysplastic syndromes and lymphoproliferative syndromes. These are the common types of cancers that may affect a pregnant woman resulting in low platelet count.
- Disseminated Intravascular Coagulation (DIC): This disease can be caused due to various pregnancy-related medical conditions. This condition may cause widespread clotting in the body. The clotting may result in low platelet count.
What further tests are required
Your doctor might ask for complete blood count initially for finding out thrombocytopenia, next is observation of the peripheral blood film. Screening for coagulation abnormalities (PT, aPTT, fibrinogen, D-dimers), liver function tests are also obtained.
Rarely, Antiphospholipid antibodies and lupus anticoagulant, and serology for systemic lupus erythematous (SLE) are done if laboratory data, history, and physical examination suggest the thrombocytopenia are secondary.
What risk can thrombocytopenia pose during pregnancy
If your platelet count is only slightly below normal, it shouldn’t cause you or your baby any problems and you won’t need any treatment. Your doctor will continue to monitor your platelet count throughout the rest of your pregnancy, in case it drops further.
Major risk thrombocytopenia poses to woman during pregnancy is: Bleeding! She is at increase danger of spontaneous oozing or bleeding from minor injuries. This risk is enhanced during C-section
When platelet counts are <70,000 per µL, many anesthesiologists hesitate to provide regional anesthesia for labor and delivery because of risk for spinal or epidural hematoma. [3]
Women should also have the blood count repeated 1-3 months after delivery to assess whether spontaneous resolution of the thrombocytopenia has occurred.
Management of Thrombocytopenia
Gestational Thrombocytopenia doesn’t require any treatment. Platelet count remains above 100,000 per µL and returns to normal after delivery. Continuous monitoring is required. Platelets count tends to fall in first and second trimester and lowest platelet counts are seen most often during the third trimester and at delivery [4].
Only treatment of Preeclampsia is to deliver the baby. Your doctor may plan your delivery sooner, considering how severe the disease is.
ITP treatment remains same with or without pregnancy, i.e. Steroids or Immunoglobulin.
How to Increase Platelet Count Naturally
You may increase your low platelet count by following natural methods:
- By including beetroot in your diet.
- By including fish and meat in your diet.
- By consuming astragalus (herb).
- By adding zinc supplements
- By consuming vitamin B-12, generally found in meat
- By consuming Vitamin K, generally found in green leafy vegetables
- By consuming chlorophyll
- By consuming Vitamin C rich food ( citrus fruits )
- By avoiding alcohol and refined sugar
It is recommended to seek your doctor’s advice before making any dietary changes.
References
- Sullivan CA, Martin JN Jr. Management of the obstetric patient with thrombocytopenia. Clin Obstet Gynecol 1995;38(3):521-534.
- Sainio S, Kekomaki R, Riikonen S, Teramo K. Maternal thrombocytopenia at term: a population-based study. Acta Obstet Gynecol Scand 2000;79(9):744-749.
- American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Practice guidelines for obstetric anesthesia: an updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia. Anesthesiology 2007;106(4):843-863.
- Robert L. Barbieri, MD reviewing Reese JA et al. N Engl J Med https://www.jwatch.org/na47033/2018/07/04/watch-out-low-platelet-counts-during-pregnancy
Image: source




 Ali Anique holds an MBBS degree from the Nishtar Medical University and currently works as a doctor at Nishtar Hospital, the biggest hospital of south Punjab province in Pakistan.
Ali Anique holds an MBBS degree from the Nishtar Medical University and currently works as a doctor at Nishtar Hospital, the biggest hospital of south Punjab province in Pakistan.