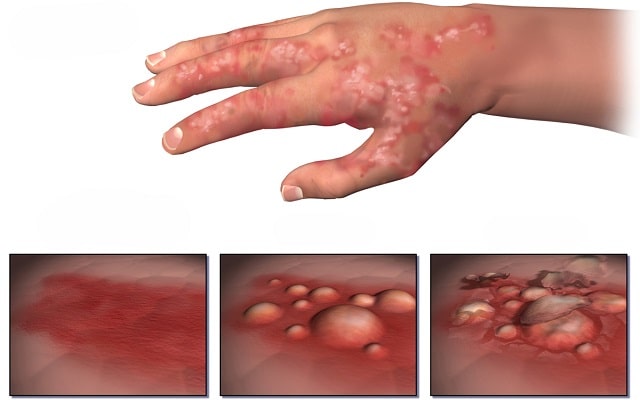
Does your toddler have red itchy skin, especially cheeks, neck, forehead or limbs which generates an irresistible urge to scratch and scratch and makes the rash even more irritated? Continue reading to know more about the disease, causes, symptoms, and management.
What is Eczema?
The terms ‘eczema’ and ‘dermatitis’ are synonymous. Eczema is a Greek word which literally means ‘to boil over’ which is exactly what happens when disease presents acutely.
Eczema is a term referring to a variety of conditions which makes the skin red, inflamed, rough, dry and cracked.
These varieties include atopic (most common), seborrhoeic, Irritant, allergic, photoallergic, chronic actinic dermatitis.
Generally, when we talk about eczema, we’re referring to its most common type: Atopic eczema, which is more explained than the other types below.
Atopic eczema: Atopy means generalized, prolonged hypersensitivity/allergy to common environmental agents such as pollen and house dust mite.
This is found in genetically predisposed individuals and your child might also have asthma, hay fever, food or other allergies.
There are strong familial associations of this disease which share the same etiology. Such kids produce excess IgE and this disease affects 1 in 10 schoolchildren.
If your child has eczema, he or she may also suffer from other atopic conditions such as Asthma and Hay Fever (Atopic Triad).
What causes Eczema?
Genetic factors are important. Epidermal barrier impairment is a major, and perhaps primary, factor in the atopic form of eczema. Mutations in the filaggrin gene have been identified as important in some [1].
Environmental factors, such as exposure to allergens in utero or during childhood, may also have an etiological role and 60–80% of individuals are genetically susceptible to the induction of IgE-mediated sensitization to environmental allergens such as food and animal hair.
Decreased skin barrier function may also allow greater penetration of allergens through the epidermis, and thus cause immune stimulation and subsequent inflammation.
One point to note here is that Eczema is not contagious. So your child didn’t get it from school or friends and he or she can be played with and loved without any fear of transmitting the disease to anyone else.
The course of Disease:
Atopic eczema usually presents with red, inflamed, crusted, raised lesion/rash whose borders are usually typically ill-defined and are extremely itchy. The distribution of rash varies with age.
In babies and infants, it is often acute and facial involvement prominent. Sometimes, a trunk is involved but the nappy area usually spared.
In toddlers and school going children, rash typically occurs in behind knees, antecubital fossae, wrists, and ankles.
In children more than 5 years of age, it appears in the folds of elbow and knee and sometimes only in hands. Around 70% of the people will only have hand eczema.[2]
How eczema would unfold itself through life is unpredictable. Some people become totally symptom-free if they identify triggering factors and adhere to treatment options recommended by the doctor.
Although dermatitis often improves age 3 or 4, exacerbations are common. While other experience flare-ups of disease with or without interventions.
What causes eczema Flare-ups?
If you or your child has eczema, it would be really important for you to know and understand the stimuli in order to live a healthy comfortable life and avoid visiting healthcare facilities repeatedly.
The following is the list of factors that can cause your symptoms to worsen, but keep in mind that not everyone would have an allergic reaction to the same factors.
- House dust mite is one the most common factor that causes an eczema flare-up
- Wool garments, nylon, and feathers.
- Dry skin
- Pet hair, pollen, molds
- Soap and other detergents, shampoos.
- Harsh chemicals and perfumes.
- Some antibacterial Ointments.
- Stress may cause exacerbations of disease and in some children, it is due to food-elimination diet.
Treatment
There is a huge impact on the social and psychological aspect of life in a child with eczema and flare-ups are common in childhood. Nevertheless, the disease becomes less severe after age 4 with fewer relapses and good control.
It is also important to identify and avoid the agents that aggravate a child’s symptoms whenever possible.
Corticosteroid creams or ointments applied thrice a day are the most effective form of treatment.
Additional use of white petroleum, saturated vegetable oil or hydrophilic petroleum gel may improve the symptoms.
These emollients also help hydrate the skin, which is important in this case as dry skin can cause itching leading to rash and lichenification. They can be applied several times a day to sore areas to help to keep the skin moist.
Prolong use of high-dose corticosteroid creams should be avoided. This will lead to systemic absorption of steroids and subsequently adrenal gland suppression.
As topical steroid side effects such as atrophy, lichenification, and darkening of skin color are most commonly feared on the face, the topical calcineurin inhibitors, tacrolimus, and pimecrolimus may be useful steroid-sparing agents in such case.
Antihistamines are not proven to be effective as sole therapy for eczema but they can be taken for symptomatic relief for complaints.
Oral Corticosteroids can be considered in resistant cases. There are best given in 2-week courses.
Precautions to take:
Having a child with eczema poses an additional responsibility on parents and child’s need for care. The above-mentioned factors for flare-ups of eczema should be avoided.
Avoidance of perfumed solutions is recommended as they may contain a substance that can cause acute symptoms.
Wool garments and nylon stuff should be avoided as this is the most common aggravating factor in children. Hygiene should be practiced and contact to house dust mite should be avoided as much as possible.
Do not let the skin of the child become dry. Moisturize frequently in winters by gentle application of creams or lotion but do not rub harshly to start an inflammatory reaction.
While in summers, try to keep the child cool as sweat can cause skin irritation and itching.
Bathing should be minimized and corticosteroid creams, emollients ointment or oils should be applied before the skin becomes dry, usually within 3 minutes, in order to have enhanced effectiveness and fewer dose requirements.
While the added stress on parents of a child with eczema is really great, most children grow out of the disease in their life while others experience relapsing-remitting course.
Appropriate knowledge and practicing the above-mentioned precautions can keep the child symptom free and live a normal healthy life.
Image source: wikimedia
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3242054/
- https://nationaleczema.org/eczema/children/
- https://kidshealth.org/en/parents/eczema-atopic-dermatitis.html




 Ali Anique holds an MBBS degree from the Nishtar Medical University and currently works as a doctor at Nishtar Hospital, the biggest hospital of south Punjab province in Pakistan.
Ali Anique holds an MBBS degree from the Nishtar Medical University and currently works as a doctor at Nishtar Hospital, the biggest hospital of south Punjab province in Pakistan.